Sleep as medicine: Functional Strategies for Deep Rest | Stockheart
Sleep disorders relief through functional medicine and nervous system care
"Your labs are normal. Try melatonin and practice better sleep hygiene."
If you're reading this, you've probably been lying awake at 3 AM wondering why your body won't let you rest, even though you're utterly exhausted. You've likely downloaded the sleep apps, bought the blackout curtains, tried every supplement on the shelf, and cut out caffeine after noon. Maybe you fall asleep fine but wake up multiple times. Or maybe you can't fall asleep at all, watching the hours tick by while your mind races through tomorrow's to-do list.
You know your body. You know this exhaustion is affecting everything—your mood, your relationships, your ability to think clearly. And you deserve more than a prescription for Ambien and a lecture about screen time. You deserve a partner who will help you understand why your nervous system won't let you rest.
The Problem: Why "Sleep Hygiene" Isn't Enough
Here's what typically happens: You tell your doctor you can't sleep. They run a basic thyroid panel (maybe), tell you your numbers are "within range," and send you home with a handout about sleep hygiene. If you're persistent, you might get a sleep study that shows nothing conclusive, or a prescription that leaves you groggy the next day but doesn't address why you can't sleep in the first place.
The conventional approach treats sleep as a behavior problem. Just do these things better, and you'll sleep. But here's what's missing: sleep isn't a behavior—it's a biological process that requires your nervous system to feel safe enough to let go.
When your sleep won't cooperate, it's not because you're not trying hard enough. It's because something deeper—in your nervous system, your biochemistry, or your body's stress response—is keeping you in a state of hypervigilance. Your body is trying to protect you by staying alert, even when there's no real threat.
But here's what we've discovered after working with hundreds of patients who've been told their insomnia is "just stress": there are specific, identifiable root causes that keep your body in a state of high alert. And when we address those causes systematically, your body remembers how to rest.
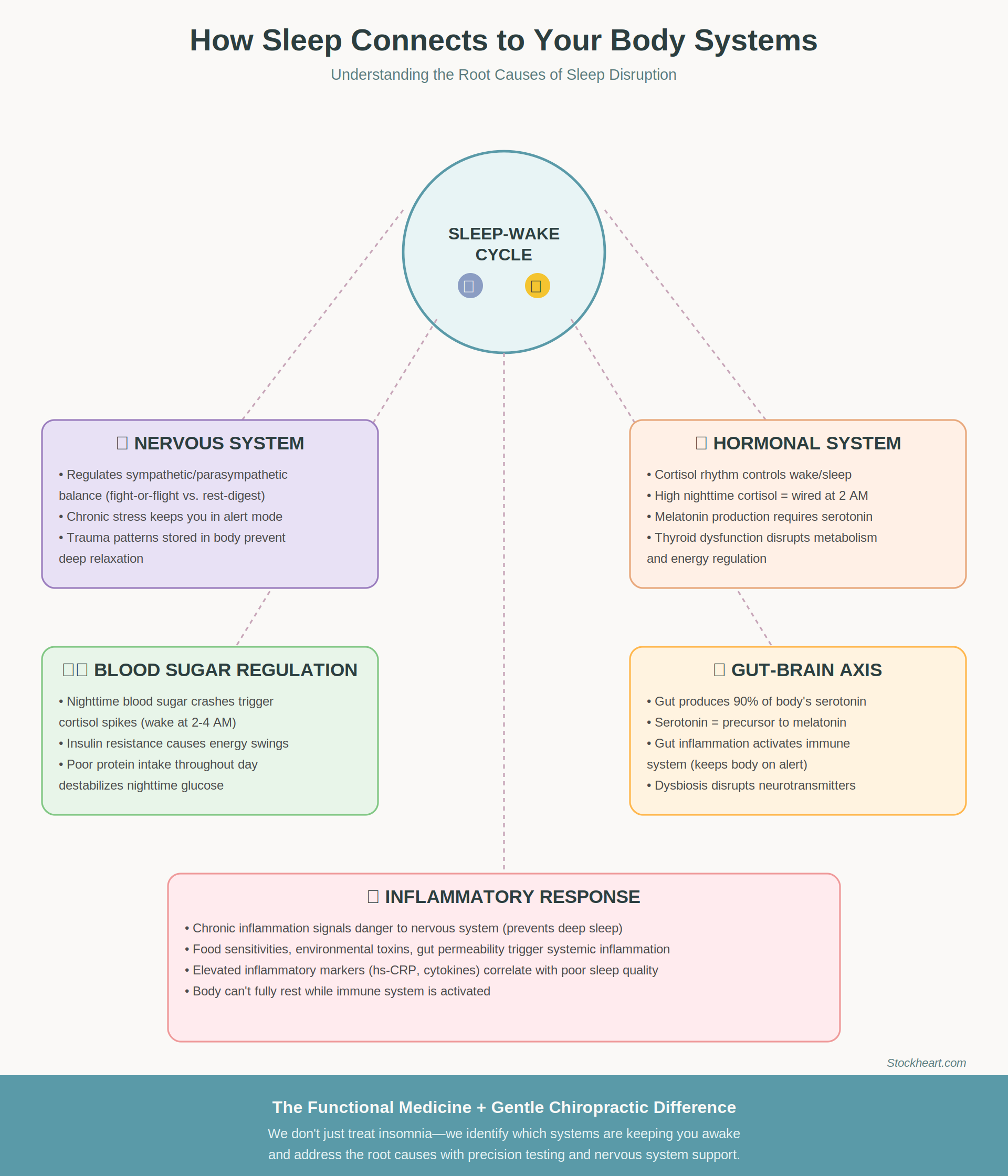
Alt text: "How sleep disorders connect to nervous system, hormones, blood sugar, gut health, and inflammation through functional medicine”
The Solution: Nervous System Safety and Biochemical Balance
At Stockheart, we approach sleep differently. We combine functional medicine's biochemical precision with DNFT chiropractic's ability to help your nervous system shift out of chronic fight-or-flight. This isn't about forcing your body to sleep—it's about removing the obstacles that are keeping you awake.
As Minnesota's dedicated gentle chiropractic and functional medicine clinic, we work with patients whose bodies are stuck in sympathetic overdrive. One of our approaches, DNFT, is uniquely effective for sleep issues because it communicates directly with your nervous system through the language it understands—subtle, specific adjustments that tell your body it's safe to down-regulate.
But nervous system work alone isn't always enough. If your cortisol rhythm is backwards, if chronic inflammation is triggering your stress response, if blood sugar crashes are waking you at 3 AM—we need to address those biochemical realities too. That's why the combination of functional medicine testing and gentle alignment of your spine creates such powerful results for sleep.
Let us show you how we identify and address the specific factors keeping you awake.
My Strategic Testing Philosophy: Start Smart, Expand Wisely
I know you've probably spent thousands of dollars on testing that told you nothing useful, or worse, that everything was "fine" when you clearly don't feel fine. I've seen patients arrive with binders full of test results and zero actionable answers.
Here's my different approach: we start with the tests most likely to reveal what's actually disrupting your sleep, then expand strategically based on what we find.
Phase 1: Foundation Testing (accessible and informative)
Comprehensive hormone panel (cortisol, DHEA, sex hormones) with 4-point cortisol curve—because cortisol rhythm is the master conductor of your sleep-wake cycle
Complete thyroid panel (not just TSH)—low thyroid function is one of the most common sleep disruptors
Blood sugar regulation markers (fasting glucose, insulin, HbA1c)—because blood sugar crashes wake you up at night
Key inflammatory markers (hs-CRP, homocysteine)—chronic inflammation keeps your nervous system on high alert
Why this matters: These tests give us a clear picture of your body's stress response, energy regulation, and inflammatory state—the three primary systems that control sleep quality. This approach typically costs $400-800 (depending on your insurance coverage) and gives us 80% of the information we need to create an effective treatment plan.
When we expand: If initial testing shows persistent inflammation, we might dig deeper into gut health. If hormone imbalances are severe, we might look at nutrient cofactors or detoxification capacity. But we only order additional testing when the initial results point us in a specific direction—not as a fishing expedition.
What's Really Keeping You Awake: The Root Causes
1. Nervous System Dysregulation: When Your Body Forgets How to Feel Safe
Your nervous system has two modes: sympathetic (active, alert, ready to respond) and parasympathetic (rest, digest, repair). Quality sleep requires your nervous system to fully shift into parasympathetic dominance. But for many people—especially those with a history of chronic stress, trauma, or ongoing life pressures—the nervous system gets stuck in a state of hypervigilance.
This isn't about "just relaxing." Your body has literally learned, often through years of needing to stay alert, that it's not safe to let go. Maybe you had years of high-stress work where you had to be "on" constantly. Maybe you went through a traumatic period where hypervigilance was adaptive. Maybe you're a parent who trained yourself to wake at every sound. Your nervous system adapted to keep you safe.
The Gentle Alignment Difference: Low-force/no-force chiropractic care works directly with your nervous system through the cranial-sacral mechanism and spinal reflexes. Unlike traditional chiropractic that uses force, DNFT uses specific directional pressure that communicates safety to your nervous system. Patients often report feeling their bodies "drop" into a deeper state of relaxation during treatment—sometimes for the first time in years. This isn't manipulation; it's communication with the part of your nervous system that controls the sleep-wake cycle.
2. Cortisol Dysregulation: The Backwards Sleep Hormone
Cortisol should follow a natural rhythm: high in the morning to help you wake up, gradually declining throughout the day, lowest at night to allow deep sleep. But chronic stress flips this pattern. You might have low cortisol in the morning (can't wake up despite sleeping), and high cortisol at night (wide awake at 2 AM despite being exhausted).
This isn't just about stress management. When your cortisol rhythm has been disrupted for months or years, your adrenal glands need specific support to reset. This might include:
Adaptogenic herbs timed to your cortisol curve
Phosphatidylserine to blunt evening cortisol spikes
Strategic protein timing to stabilize blood sugar and support healthy cortisol rhythms
Nervous system work through DNFT to reduce the chronic stress signal driving cortisol dysregulation
The key is testing your actual cortisol pattern (through saliva or dried urine testing) rather than guessing. What works for high cortisol at night makes low cortisol in the morning worse—we need precision here.
3. Blood Sugar Instability: The 3 AM Wake-Up Call
If you wake up between 2-4 AM most nights, especially with your heart racing or feeling anxious, blood sugar dysregulation is likely involved. Here's what happens: Your blood sugar drops too low during the night, triggering a cortisol surge to raise it back up. That cortisol spike wakes you up.
This pattern often develops in people who:
Skip breakfast or eat carb-heavy breakfasts
Go too long between meals during the day
Eat dinner early and nothing before bed
Have insulin resistance or pre-diabetes
Under-eat protein throughout the day
The solution isn't just a bedtime snack (though that might help). It's addressing insulin sensitivity during the day, ensuring adequate protein intake, and sometimes using specific nutrients like chromium or berberine to support healthy blood sugar regulation.
4. Gut-Brain Axis Disruption: The Hidden Connection
Your gut produces more serotonin than your brain—and serotonin is the precursor to melatonin, your primary sleep hormone. When gut health is compromised through dysbiosis, inflammation, or increased intestinal permeability, your body's ability to produce adequate sleep-promoting neurotransmitters is impaired.
Additionally, gut inflammation triggers systemic inflammation, which activates your immune system and keeps your nervous system in a state of alert. You can't sleep deeply when your body thinks it's fighting an infection.
Signs your gut might be disrupting your sleep:
Digestive issues (bloating, irregular bowel movements, food sensitivities)
Waking up with night sweats
Vivid, disturbing dreams
Difficulty staying asleep even when falling asleep is easy
Addressing gut health often requires a systematic approach: removing inflammatory triggers, supporting the gut barrier, replenishing beneficial bacteria, and addressing any underlying infections or imbalances.
Alt text: "Comprehensive functional medicine assessment and gentle chiropractic treatment"
Sarah's Story: From Exhausted to Restored
Sarah came to me after two years of severe insomnia. She was a 42-year-old executive who had always been a good sleeper until a particularly stressful work period coincided with perimenopause. What started as occasional sleepless nights became a chronic pattern—lying awake for hours, finally falling asleep around 4 AM, then dragging herself through the day on coffee and willpower.
She'd tried everything: Ambien (which worked initially but left her feeling "drugged"), cognitive behavioral therapy for insomnia (helped with anxiety about sleep but didn't restore actual sleep), acupuncture (felt relaxing but no lasting change), and an ever-growing supplement routine that cost hundreds of dollars monthly with minimal results.
What we discovered: Sarah's 4-point cortisol test showed sky-high nighttime cortisol and depleted morning cortisol—a complete reversal of the healthy pattern. Her comprehensive thyroid panel revealed subclinical hypothyroidism (TSH was "normal" at 3.8, but Free T3 was low). Her fasting insulin was elevated, indicating insulin resistance that was causing blood sugar crashes at night.
Our approach: We started with twice-weekly non-force treatments to help her nervous system downregulate. Within three sessions, she noticed her body felt "less buzzy" at night. We added phosphatidylserine to blunt her evening cortisol spike, supportive adaptogens for her depleted morning cortisol, and thyroid support to optimize her metabolism. We implemented a strategic eating schedule with adequate protein to stabilize blood sugar.
The timeline: Within three weeks, Sarah was falling asleep within 30 minutes most nights. By two months, she was sleeping 6-7 hours consistently and waking feeling rested. At six months, her cortisol rhythm had normalized, and she described her sleep as "better than it's been in a decade."
Key insight: Sarah's body wasn't broken—it was stuck in a protective pattern that served her during that high-stress period but never turned off. Once we addressed both the nervous system signaling and the biochemical imbalances, her body remembered how to rest.
What Working Together Looks Like
Discovery Session: Testing the Waters
We start with a 20-minute discovery call. This isn't a sales pitch—it's a genuine conversation where I learn about your sleep challenges and you get to feel whether this approach resonates with you. Many patients have been through so many failed attempts that they need to know there's a real plan before committing. I get it. We'll discuss your symptoms, what you've already tried, and whether functional medicine + DNFT is likely to be helpful for your specific situation.
Comprehensive 90-Minute Intake: The Deep Dive
If we both agree we're a good fit, your first appointment is where the real work begins:
Complete health history: We map your entire timeline—when did the sleep issues start, what else was happening in your life and body, what's been tried and what helped (even a little). The patterns matter.
Neurological assessment: I evaluate your nervous system's ability to regulate itself—how your body responds to stress, where you're holding tension, how your cranial-sacral mechanism is functioning.
Orthopedic examination: We assess structural factors that might be contributing—neck tension, jaw dysfunction (TMJ is a huge sleep disruptor), spinal alignment issues.
First gentle chiropractic treatment: You experience the work immediately. Most patients describe it as deeply relaxing, often feeling their nervous system "drop" into a state they haven't accessed in years.
We discuss testing strategy and create your initial treatment plan before you leave.
Ongoing Partnership
This isn't a quick fix, but it's also not endless treatment. We commit to giving you a timeline with milestones. This ensures we are aligned in our goals and expectations. Most sleep patients see significant improvement within 4-8 weeks with consistent nervous system support through DNFT (typically starting at 2x/week, then spacing out) combined with targeted functional medicine interventions based on your test results.
We track your progress carefully—sleep quality, time to fall asleep, number of wake-ups, morning energy—and adjust our approach based on what's working. Some patients achieve stable sleep and transition to monthly maintenance. Others discover that addressing their sleep reveals deeper health patterns worth exploring.
You're in charge of your care. We move at your pace, with your budget and life circumstances in mind.
Alt text: "Woman thriving after addressing sleep disorder root causes"
Ready to Sleep Again?
If you're exhausted from being exhausted—if you're done with band-aid solutions that don't address why your body won't let you rest—let's talk.
Choose Your Next Step:
-
Let's have a real conversation about your sleep challenges. No pressure, no sales pitch—just an honest discussion about whether this approach makes sense for you. [Schedule your discovery call]
-
If you already know this resonates and you're ready to dive in, book your intake appointment. We'll do your complete assessment, first gentle treatment, and create your testing strategy in one appointment. [Book your intake]
-
Not ready to book yet? Get my free guide that walks through the specific tests and biomarkers that reveal why you can't sleep—and what to do about them. [Download the free guide]
Your body wants to sleep. It's designed for deep, restorative rest. When it can't, there's always a reason. Let's find yours.
Dr. Michele Renee DC, Founder of Minnesota's Leading Integrative Gentle Chiropractic Practitioner
Stockheart: Functional Medicine + Nervous System Care
Your body wants to sleep. It's designed for deep, restorative rest. When it can't, there's always a reason. Let's find yours.